Reducing the Transmission of Viruses with Humidification Part 2: Understanding Airborne Viruses
/By Chad Edmondson
The World Health Organization (WHO) made big news in early July by acknowledging increasing scientific evidence that COVID-19 (SARS- CoV-2) bears the risk of airborne transmission. But wait -- didn’t we already know that? The answer to that question is more complicated than one might think. Just because someone catches a virus from inhaling droplets in an infected person’s sneeze doesn’t mean the virus is “airborne.”
When scientists and health professionals talk about airborne viruses, they are not talking about those contained in the expelled droplets of a cough or sneeze, but those that remain viable in a cloud of much smaller droplets that can float around in the air for several minutes or even hours after the infected person has left the room. At 5 microns or less (about one tenth of the diameter of a human hair), these droplets are no longer referred to as droplets, but “aerosols.” They not only linger in the air longer; they can travel distances well beyond the 6 ft. social distancing benchmark. When a virus can be carried and remain viable in such a small particle of gas, it is considered to be airborne.
A whole host of viruses are known to be airborne, including rhinovirus (common cold), influenza (type A, type B, H1Nq, and chickenpox, among others. It has been well established (if not formally acknowledged) that Covid-19 is also part of this highly infectious club.
How Humidity Impacts Airborne Viruses
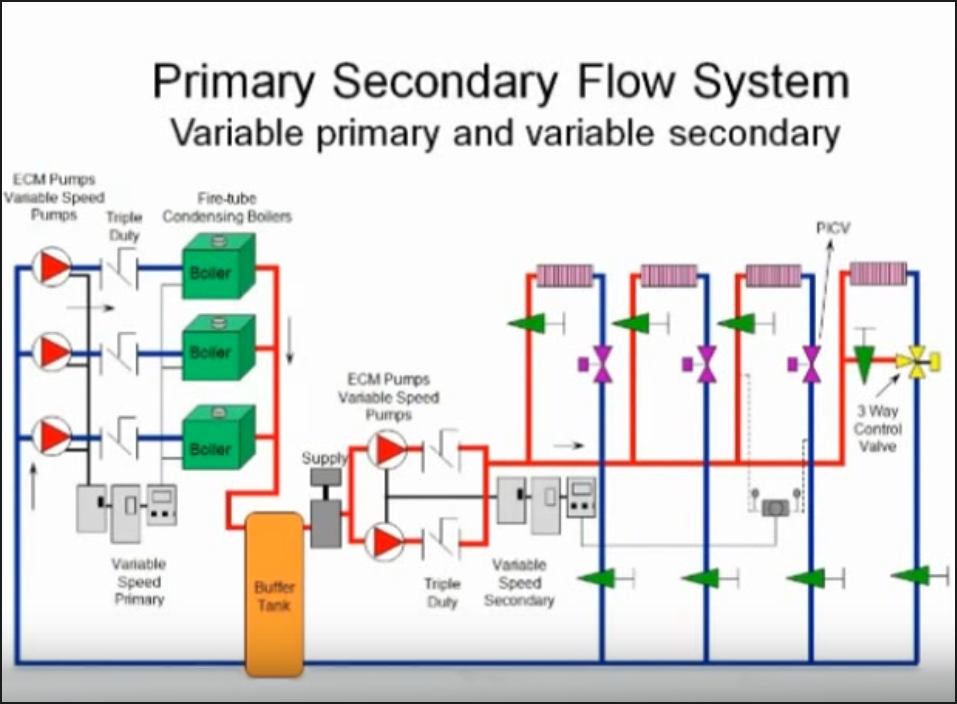
The smaller the aerosol droplets the more problematic they can be. Larger, heavier droplets tend to travel only a few feet from an infected person’s nose or mouth before succumbing to gravity and falling to the floor or underlying surface. But researchers have verified that airborne pathogens can travel up to 25 feet from a sneeze. Research has shown that depending on their size and the environment, they can remain suspended in the air for up to two or more days (Figure 1). This makes it much more difficult to mitigate a virus with masks and social distancing alone, particularly when it comes to enclosed and densely populated spaces like schools, offices and hospitals.
These smaller droplets or particles not only last longer and travel further, they become more lethal because they can be inhaled more deeply into the lungs and pulmonary system.
Humidity (or the lack thereof) impacts airborne viruses in two ways. First, when air is very dry (40% RH or below), the moisture in droplets evaporate more quickly. But the droplets don’t go away – they just get smaller and smaller, remaining airborne for longer periods of time and traveling greater distances. When and if they are inhaled, subsequently infecting someone new, dry air makes is harder for the body to expel the virus through its natural defenses. Specifically, low humidity thickens respiratory mucus, which impairs the ability of small cellular protrusions called cilia to move the mucus and help clear pathogens.[1]
Of course, high humidity can also help spread viruses. As discussed in the previous blog, the sweet spot for indoor RH is 40 to 60%.
[1] https://medium.com/datadriveninvestor/fighting-the-flu-with-humidity-28d4ccb42bd7